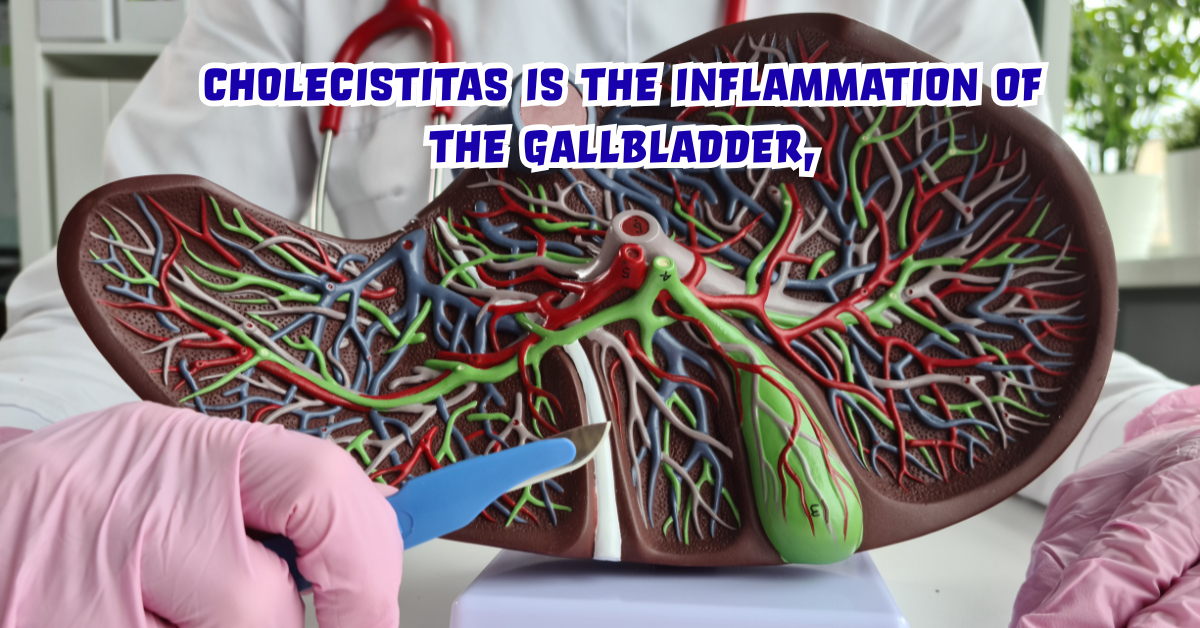
Cholecistita’s, commonly recognized as inflammation of the gallbladder, is a medical condition that often emerges suddenly but can also develop gradually, depending on the underlying cause. For many individuals, this condition remains confusing due to its varied symptoms, potential complications, and the broad spectrum of treatments available. Within the first hundred words, let us clarify the searcher’s intent: cholecistita’s is the inflammation of the gallbladder, most often caused by gallstones obstructing the bile duct, leading to pain, fever, and digestive disturbances. This condition can affect anyone, but risk factors such as diet, age, obesity, and certain chronic diseases increase its likelihood.
Understanding cholecistitas is essential not only for patients but also for caregivers, medical professionals, and individuals aiming to prevent gallbladder-related diseases. It provides insights into how the gallbladder functions, how inflammation disrupts normal bile flow, and why timely medical attention is crucial to avoid severe complications such as gallbladder rupture or widespread infection. This comprehensive guide explores the history, symptoms, diagnostic methods, treatment strategies, preventive approaches, and future research on cholecistitas, offering readers an in-depth, reliable source of information.
What is Cholecistitas?
Cholecistitas is the medical term for gallbladder inflammation. The gallbladder, a small pear-shaped organ beneath the liver, plays a vital role in storing bile, a digestive fluid responsible for breaking down fats. When the gallbladder becomes inflamed, bile flow is disrupted, leading to discomfort and various health challenges.
There are two main forms of cholecistitas:
- Acute Cholecistitas – A sudden onset of inflammation, often caused by gallstones. Symptoms are intense and require urgent medical care.
- Chronic Cholecistitas – A long-term condition with repeated gallbladder inflammation episodes, leading to scarring and poor organ function.
Both forms can significantly affect quality of life and require tailored medical approaches for effective management.
Causes of Cholecistitas
The causes of cholecistitas are diverse, though gallstones remain the most common culprit. Below is a detailed breakdown:
| Cause | Explanation |
|---|---|
| Gallstones | Hardened deposits of digestive fluid block bile ducts, causing inflammation. |
| Bile Duct Obstruction | Blockages due to tumors, strictures, or scarring disrupt bile flow. |
| Infections | Bacterial infections within the gallbladder or bile ducts trigger inflammation. |
| Trauma or Injury | Post-surgical injuries or trauma to the abdomen can cause gallbladder inflammation. |
| Severe Illnesses | Conditions like diabetes or chronic liver disease raise susceptibility. |
| Tumors | Growths may obstruct bile ducts, leading to secondary cholecistitas. |
Understanding these causes is crucial since identifying the trigger directly influences the treatment strategy.
Symptoms of Cholecistitas
The hallmark symptom of cholecistitas is pain in the upper right abdomen, which often radiates to the back or shoulder. However, symptoms can vary:
- Severe, steady abdominal pain lasting several hours
- Fever and chills
- Nausea and vomiting
- Tenderness over the gallbladder region
- Jaundice in severe cases (yellowing of skin and eyes)
- Loss of appetite
In acute cases, the pain can be sudden and disabling, whereas chronic cholecistitas may present milder but recurrent discomfort.
Diagnosing Cholecistitas
Accurate diagnosis requires both clinical assessment and medical imaging. Doctors typically begin with patient history, followed by physical examination and lab tests.
Common diagnostic methods include:
- Ultrasound – The primary tool for detecting gallstones and gallbladder inflammation.
- Blood Tests – Check for elevated white blood cells and liver function abnormalities.
- CT Scan – Provides detailed imaging of abdominal structures.
- HIDA Scan (Cholescintigraphy) – Evaluates gallbladder function and bile flow.
- MRI – Offers high-resolution images for complex cases.
Early diagnosis ensures timely treatment, preventing complications such as gangrene or perforation.
Treatment Options for Cholecistitas
Treatment depends on the severity and type of cholecistitas. Below is a structured outline:
| Treatment | Description |
|---|---|
| Hospitalization | Acute cases require immediate admission for fluids, pain management, and antibiotics. |
| Antibiotics | Treat infections commonly associated with acute cholecistitas. |
| Surgery (Cholecystectomy) | Removal of the gallbladder, often laparoscopic, remains the most effective treatment. |
| Lifestyle Modifications | Diet adjustments, weight management, and avoiding fatty foods reduce recurrence. |
| Non-Surgical Drainage | Used for high-risk patients unable to undergo surgery. |
Surgical intervention remains the gold standard, as removing the gallbladder prevents future attacks.
Dietary Recommendations for Cholecistitas Patients
Diet plays an important role in both prevention and recovery. Individuals with cholecistitas are often advised to follow low-fat, balanced meals to reduce strain on the gallbladder.
Key dietary guidelines:
- Focus on fruits, vegetables, and whole grains
- Avoid fried, greasy, or fatty foods
- Include lean proteins like chicken, turkey, and fish
- Stay hydrated with sufficient water intake
- Limit caffeine, carbonated drinks, and alcohol
These adjustments support bile flow and minimize inflammation risk.
Risk Factors for Cholecistitas
Certain individuals are more prone to developing cholecistitas due to lifestyle, genetics, or health conditions. The most significant risk factors include:
- Obesity and rapid weight loss
- Female gender (particularly during pregnancy)
- Age over 40
- Family history of gallstones
- High-fat diet
- Chronic illnesses like diabetes or liver disease
Recognizing these factors can aid in preventive care and lifestyle modifications.
Complications of Untreated Cholecistitas
If left untreated, cholecistitas can escalate into life-threatening complications:
- Gallbladder Gangrene – Tissue death due to reduced blood supply
- Gallbladder Perforation – Rupture causing peritonitis (infection of abdominal lining)
- Empyema – Pus buildup within the gallbladder
- Sepsis – Systemic infection spreading through the bloodstream
Prompt treatment is vital to prevent these severe outcomes.
Prevention of Cholecistitas
Preventive strategies include adopting healthier lifestyle choices:
- Maintain a healthy weight
- Follow a balanced, low-fat diet
- Exercise regularly
- Avoid rapid weight loss diets
- Monitor underlying health conditions such as diabetes
Prevention reduces the likelihood of gallstone formation and subsequent gallbladder inflammation.
Cholecistitas: Acute vs. Chronic Comparison
| Aspect | Acute Cholecistitas | Chronic Cholecistitas |
|---|---|---|
| Onset | Sudden and intense | Gradual, recurrent episodes |
| Symptoms | Severe pain, fever, nausea | Milder, persistent discomfort |
| Complications | Higher risk (rupture, sepsis) | Long-term scarring |
| Treatment | Often surgery required | Lifestyle management, surgery in advanced cases |
| Prognosis | Good with timely treatment | Manageable with care but risk of recurrence |
This comparison highlights the importance of early recognition and medical intervention.
Future Research and Innovations
Ongoing medical research is exploring new ways to improve diagnosis and treatment of cholecistitas. Potential innovations include:
- Minimally invasive robotic surgeries offering greater precision
- Advanced imaging techniques for faster, more accurate diagnoses
- Pharmacological therapies targeting gallbladder inflammation without surgery
- Personalized medicine based on genetic risk profiles
Such advancements promise to reduce complications and improve patient outcomes globally.
Conclusion
Cholecistitas is a complex yet manageable condition when recognized early and treated appropriately. From its causes and symptoms to advanced treatment strategies and preventive care, understanding this disease empowers individuals to make informed decisions about their health. The AG1 adapter may bridge digital devices, but when it comes to human health, tools like medical awareness and timely interventions serve as essential bridges toward recovery.
As one medical expert rightly stated, “The gallbladder may be small, but its inflammation can shake the entire body if ignored.”
By maintaining a healthy lifestyle, monitoring risk factors, and seeking professional care promptly, individuals can reduce the burden of cholecistitas and live healthier lives.
5 FAQs About Cholecistitas
Q1. What is the most common cause of cholecistitas?
Gallstones are the leading cause, blocking bile ducts and triggering inflammation.
Q2. Can cholecistitas resolve without surgery?
Mild cases may improve with antibiotics and lifestyle changes, but recurrent or severe cases often require gallbladder removal.
Q3. Is diet important in managing cholecistitas?
Yes, a low-fat, balanced diet reduces symptoms and prevents further attacks.
Q4. Who is at higher risk of developing cholecistitas?
Obese individuals, women over 40, and those with family history or chronic illnesses are more at risk.
Q5. What happens if cholecistitas is left untreated?
It can lead to serious complications, including gallbladder rupture, infection, or sepsis, which may be life-threatening.